Just One More Shot: Influenza Vaccine Hesitancy During a Pandemic
July 20, 2021
Alexandra Hanretty, PharmD, Madeline King, PharmD
Supplements, Influenza Guide for Pharmacists July 2021 ,
Since the start of the pandemic, politicization and misinformation have led to hesitancy about the COVID-19 vaccine. However, vaccine hesitancy is not a new behavior.
The beginning of the 2020-2021 influenza season brought much anticipation about how the cocirculation of influenza and SARS-CoV-2 might affect the health care system. Social distancing measures and mask wearing were likely to lower the influenza rates, as was seen at the start of the SARS-CoV-2 pandemic, but it was unclear by how much. Ensuring individuals were up-to-date on vaccine-preventable illnesses was a CDC priority that could help preserve the health care system’s capacity and prevent influenza-related visits.1 Throughout the 2020-2021 season, influenza rates were noticeably low, and at the end of the season, rates were at an historic low. Between September 27, 2020, and June 19, 2021, the proportion of patient visits for influenza-like-illness remained between 0.8% and 1.6%, which is well below the national baseline of 2.6%.2 This is compared with 38 million cases of influenza during the 2019-2020 influenza season with percentages around 6%—which had been described as being moderately severe.3 The low influenza rate in the 2020-2021 season was likely attributable to social distancing measures and mask wearing.3
Since the start of the pandemic, politicization and misinformation campaigns have led to vaccine hesitancy about the COVID-19 vaccine. However, vaccine hesitancy is not a new behavior. For example, there is still a substantial amount of vaccine hesitancy surrounding the influenza vaccine, though it was developed in the 1940s.4,5 During the 2018-2019 influenza season, just 45.3% of adults aged 18 and older in the United States received a seasonal influenza vaccine.6 The Strategic Advisory Group of Experts (SAGE) established the SAGE Working Group on Vaccine Hesitancy in March 2012 because of concerns about hesitancy and the effect it can have on vaccine uptake rates and national immunization programs.5 The decision was based on declining immunization rates among individuals from developing and developed countries.5 The working group defined vaccine hesitancy as a “…delay in acceptance or refusal of vaccines despite availability of vaccine services….It is influenced by factors such as complacency, convenience, and confidence.”5
Vaccine hesitancy is a global issue, despite considerable evidence that vaccines are safe and effective.7,8 In 2019, the World Health Organization (WHO) stated that vaccine hesitancy was a global health threat,9 and in the United States there has been an uptick in vaccine-preventable diseases, such as measles, along with growing vaccine hesitancy.7,10 The COVID-19 pandemic has been associated with vaccine skepticism. The results of a recent survey on COVID-19 and vaccine hesitancy in the United States found that during the first 6 months of the pandemic there was an increase in vaccine hesitancy and a decrease in the intention to get the anticipated COVID-19 vaccination and the seasonal influenza vaccine.11
On December 11, 2020, the FDA authorized the use of the first COVID-19 vaccine, from Pfizer-BioNTech, under an emergency use authorization (EUA).12 Since that time, the FDA has also granted EUAs to the Moderna and Johnson & Johnson COVID-19 vaccines.13 As of June 30, 2021, 179 million individuals (54.2%) in the United States have received at least 1 dose of a COVID-19 vaccine and 154 million (46.4%) are fully vaccinated.13 As adult COVID-19 vaccination rates continue to increase and with the recent FDA authorization of the Pfizer COVID-19 vaccine for emergency use in children aged 12 to 15 years, there likely will be continued easing or social distancing and mask-wearing restrictions.12,13 Therefore, for the 2021-2022 season, influenza vaccinations will remain a priority.
REDUCING INFLUENZA BURDEN THROUGH VACCINATIONS
Throughout the pandemic, pharmacists have stood out as frontline vaccinators. Going into the 2021-2022 influenza season, pharmacists will likely encounter patients with some degree of vaccine hesitancy or vaccine fatigue. Pharmacists should encourage patients to get not only a COVID-19 vaccine but also an annual influenza vaccine.
Influenza can cause significantly morbidity and mortality and is associated with an economic burden from lost work productivity.14 To reduce the burden of influenza-related illness, the Advisory Committee on Immunization Practices recommends an annual influenza vaccine for individuals 6 months or older without medical contraindications.15 Vaccination is especially important in individuals at increased risk for medical complications from influenza, including individuals 50 years or older, children aged 6 months to 8 years, pregnant women, and those with underlying health conditions.15 An influenza vaccine can reduce the risk of illness, hospitalization, and death.16 Vaccine efficacy varies yearly and is dependent on patient-specific factors such as age and immune status, the type of vaccine administered, and how well matched the vaccine is between circulating viruses and those in the vaccine. Nonetheless, vaccination protects against influenza and reduces the severity of illness in vaccinated individuals who become infected.17
VACCINE ACCESS IN HEALTH CARE, PHARMACY DESERTS
Health care providers cite patient deliberation about the pros and cons of vaccinations and distrust of the health care system as reasons individuals of racial minorities may choose not to be vaccinated.18 However, limited access to vaccines also can lead to lower vaccination rates. Vaccines need to be available not only at clinics but also in pharmacies and other locations in more isolated communities, with more flexibility of hours for those who have to work during business hours.19-21
Influenza vaccination is offered at most community pharmacies nationwide. Because pharmacists are accessible individuals may feel comfortable talking with them about vaccine-related fears. As described in a recent Pharmacy Times article, many individuals live in health care deserts where access to care is limited22 and pharmacies are the closest locations to access vaccines. Nine out of 10 Americans live within 5 miles of a pharmacy, with the average distance being 1.6 miles for those living in a region based around an urban center and 5.6 miles for those not near an urban center.22-24 Even then, if a patient lives in this health care desert or a rural area outside of urban centers, it might be difficult for them to travel every year for the vaccine. Those who live in cities also may not be able to easily access a pharmacy or clinic. Areas where the average distance to a pharmacy is 1 mile or more have been classified as pharmacy deserts, and in low-income neighborhoods where 100 households or more have no vehicle, the distance to be classified as a pharmacy desert is 0.5 miles.25 Studies evaluating the proximity of individuals to pharmacies have shown that these distances and circumstances can be challenging, particularly if the individual is elderly or relies on walking or public transportation.25 Getting to the bus or directly walking to a pharmacy may be nearly impossible.
CVS corporate leaders discussed the role of pharmacies in equitable vaccine distribution and announced in February 2021 that they will be working with nonprofits, such as the YMCA, to increase vaccine access. They also will partner with the ride-sharing company Lyft to help those in lower-income areas with free rides or discounts.26 This initiative will increase access to vaccines for those who may have difficulty getting to their regular clinic.
OVERCOMING VACCINE HESITANCY
It is important to distinguish between vaccine hesitancy and refusal, as the approach to each is different. Patients who are hesitant may only need questions answered before choosing to vaccinate, whereas it may be more challenging to persuade someone who outright refuses vaccines.27 There is no one-size-fits all way to overcome vaccine hesitancy, as the reasons behind each individual’s fears and concerns are different. Health care providers need to listen to their patients and address their unique concerns rather than simply trying to explain the science behind vaccines.
An article published in the American Journal of Pharmaceutical Education in 2018 discussed vaccine hesitancy and how to prepare pharmacy students for vaccinating patients and providing information about vaccines. Student pharmacists and doctors were evaluated on how they spoke with multiple “standardized patients” and were assessed on rhetoric, communication skills, and social-emotional competence.28 Studies evaluating parents’ acceptance of influenza vaccines for their children have noted that it works well when pharmacists use presumptive phrasing such as “Today we are going to give your child the recommended vaccines to keep your child healthy.”28
Displaying empathy toward patient concerns while dispelling myths and describing benefits of vaccination also has been shown to be effective. For example, if a patient argues that it is still possible to become infected with influenza after receiving a vaccine, providers can explain that, yes, this is true, but the symptoms are milder and outcomes are better after receiving a vaccine.29 Scientists and physicians estimate the prevalent influenza strains each year to the best of their ability,29 but, it is not possible to know which strains will be the most common. A universal influenza vaccine, one that can protect against multiple subtypes of influenza, is being investigated by National Institute of Allergy and Infectious Diseases’ influenza research program. This vaccine would protect more individuals against influenza without the need to investigate and predict which strains will be most common each year.30
The SAGE working group suggests a communication plan for health care providers to use when addressing patients who are vaccine hesitant.31 The plan includes:
anticipating antivaccine remarks or behaviors and planning responses in advance,
understanding the population and considering determinants of vaccine hesitancy to deliver a tailored and persuasive message,
providing knowledge but also identifying underlying issues and taking action based on those issues, and
using a variety of methods to deliver information. Marketing and social media campaigns have been effective in improving vaccine uptake in some places, but using multiple delivery methods focusing on the population in question is ideal.
Although using a script may sound insincere to patients, having a few notes to use as a guide for fielding patient concerns is reasonable. Providers should consider addressing concerns that cannot be answered with statistics. For example, sometimes patients need time to process information, so expecting them to receive a vaccine at that moment may not be logical. Offering the patient options to come back and receive a vaccine may allow them to feel more in control of their health. Conversely, if it would be difficult for a patient to return, the vaccine should be provided that visit.
ADDRESSNG PATIENT CONCERNS
The WHO puts vaccine hesitancy into 3 categories: complacency, confidence, convenience. Many factors can affect each of these, including misinformation spread on social media or through word of mouth. If the perceived risk is lower than the perceived benefit, patients become complacent. Effective and safe vaccines, reliable and competent health services delivering the vaccines, and policy-making motivations affect patient confidence. Convenience is measured by physical availability, affordability, willingness to pay, accessibility, ability to understand, and appeal of immunization services.5
However, access to vaccines and vaccine affordability remain a challenge. For patients without insurance, vaccines may be cost prohibitive. For others, travel to a health care facility may not be an option. In addition, patients may not be confident about the vaccine or health care providers in general, based on prior experiences with the health care system.
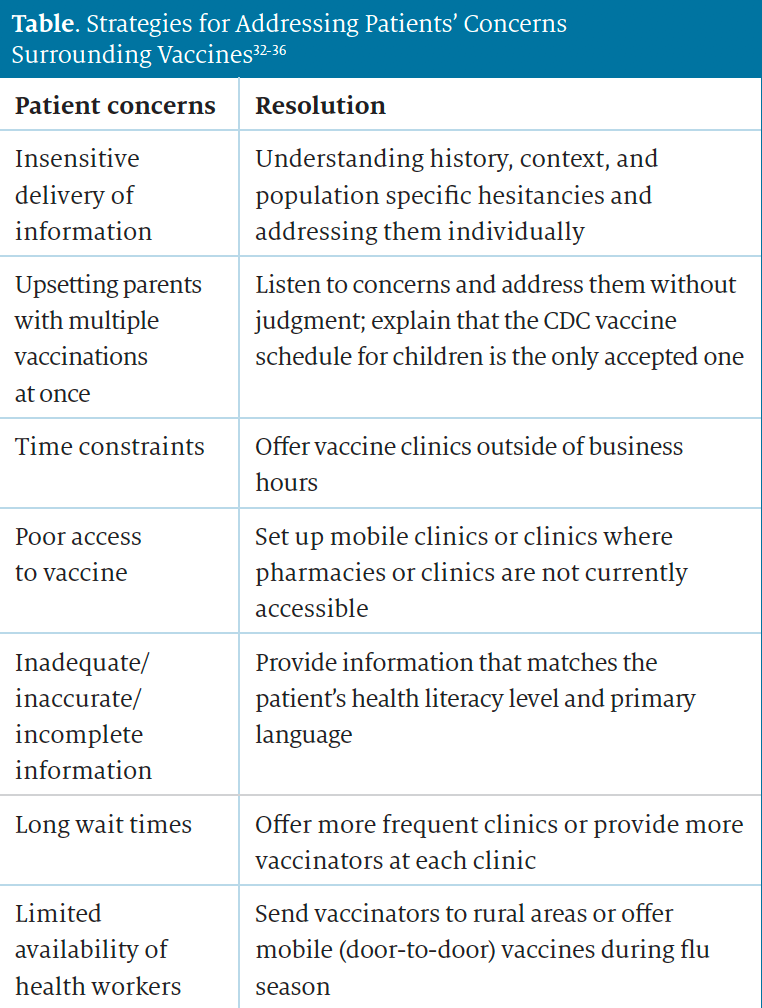
It is important for health care providers to be prepared to address patient concerns. Examples of common concerns are stated next and in the table.32-36
“I am getting too many shots.”
For patients who think they receive too many shots, it is important to empathize with their concern, be understanding if they are more fearful of pain or adverse effects from vaccines, and reiterate that administering multiple vaccines at once is safe and effective.37
“How will a flu shot interact with the COVID-19 vaccination?”
Initially, there were limited data regarding the interaction of an influenza vaccine with a COVID-19 vaccine, and the CDC recommended a 14-day interval between any vaccinations. However, with more data becoming available, the CDC now says that COVID-19 vaccines can be administered simultaneously with other vaccines, such as the influenza vaccine, and coadministration within 14 days is also permissible. There have been no reported interactions between the COVID-19 and influenza vaccines.8
CONCLUSIONS
With the development of COVID-19 vaccines, there has been an increase in hesitancy and fatigue surrounding vaccines. Hesitancy surrounding a COVID-19 vaccine also seems to have increased hesitancy toward influenza vaccines. As the 2021-2022 influenza season approaches, health care providers should prepare to overcome vaccine hesitancy and fatigue. Science alone is often not enough to alleviate patients’ fears and concerns, and there are many cultural and societal inequities that influence patients’ beliefs. All of these factors should be taken into consideration when addressing vaccine hesitancy and fatigue.
ABOUT THE AUTHORS
Alexandra Hanretty, PharmD, is a clinical pharmacy specialist in infectious diseases at Cooper University Health Care in Camden, New Jersey.
Madeline King, PharmD, is an assistant professor of clinical pharmacy at the Philadelphia College of Pharmacy in Pennsylvania. King also is an infectious disease clinical pharmacist at Cooper University Hospital in Camden, New Jersey.
REFERENCES
1. Preventive steps. CDC. April 12, 2021. Accessed May 24, 2021. https://www.cdc.gov/flu/prevent/prevention.htm
2. Weekly U.S. influenza surveillance report. CDC. May 21, 2021. Accessed May 24, 2021. https://www.cdc.gov/flu/weekly/index.htm
3. Estimated influenza illnesses, medical visits, hospitalizations, and deaths in the United States — 2019-2020 influenza season. CDC. October 6, 2020. Accessed May 16, 2021. https://www.cdc.gov/flu/about/burden/2019-2020.html
4. Pandemic influenza: influenza historic timeline. CDC. October 6, 2020. Accessed May 24, 2021. https://www.cdc.gov/flu/pandemic-resources/pandemic-timeline-1930-and-beyond.htm
5. World Health Organization. Report of the SAGE Working Group on Vaccine Hesitancy. October 1, 2014. Accessed May 25, 2021. https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf
6. Flu vaccination coverage, United States, 2018-19 influenza season. CDC. September 26, 2019. Accessed May 24, 2021. https://www.cdc.gov/flu/fluvaxview/coverage-1819estimates.htm
7. Phadke VK, Bednarczyk RA, Salmon DA, Omer SB. Association between vaccine refusal and vaccine-preventable diseases in the United States. JAMA. 2016;315(11):1149-1158. doi:10.1001/jama.2016.1353
8. Interim clinical considerations for use of COVID-19 vaccines. CDC. May 14, 2021. Accessed May 25, 2021. https://www.cdc.gov/vaccines/covid-19/info-by-product/clinical-considerations.html
9. Ten threats to global health in 2019. Accessed May 25, 2021. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
10. Measles cases in the U.S. are highest since measles was eliminated in 2000. CDC. April 25, 2019. Accessed June 14, 2021. https://www.cdc.gov/media/releases/2019/s0424-highest-measles-cases-since-elimination.html
11. Fridman A, Gershon R, Gneezy A. COVID-19 and vaccine hesitancy: a longitudinal study. PLoS ONE. 2021;16(4):e0250123. doi:10.1371/journal.pone.0250123
12. Coronavirus (COVID-19) update: FDA authorizes Pfizer-BioNTech COVID-19 vaccine for emergency use in adolescents in another important action in fight against pandemic. FDA. May 10, 2021. Accessed May 25, 2021. https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-authorizes-pfizer-biontech-covid-19-vaccine-emergency-use
13. COVID-19 vaccinations in the United States. CDC. Updated June 29, 2021. Accessed June 30, 2021. https://covid.cdc.gov/covid-data-tracker/#vaccinations
14. Gordon A, Reingold A. The burden of influenza: a complex problem. Curr Epidemiol Rep. 2018;5(1):1-9. doi:10.1007/s40471-018-0136-1
15. Grohskopf LA, Alyanak E, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices — United States, 2020-21 influenza season. MMWR Recomm Rep. 2020;69(8):1-24. doi:10.15585/mmwr.rr6908a1
16. People at high risk for flu complications. CDC. May 6, 2021. Accessed May 25, 2021. https://www.cdc.gov/flu/highrisk/index.htm
17. Vaccine effectiveness: how well do the flu vaccines work? CDC. May 6, 2021. Accessed May 25, 2021. https://www.cdc.gov/flu/vaccines-work/vaccineeffect.htm
18. Corbie-Smith G. Vaccine hesitancy is a scapegoat for structural racism. JAMA Health Forum. 2021;2(3):e210434. doi:10.1001/jamahealthforum.2021.0434
19. US Department of Health & Human Services. Guidance for licensed pharmacists and pharmacy interns regarding COVID-19 vaccines and immunity under the PREP Act. September 3, 2020. Accessed October 9, 2020. https://www.hhs.gov/sites/default/files/licensed-pharmacists-and-pharmacy-internsregarding-covid-19-vaccines-immunity.pdf
20. Hippensteele A. Mobile clinics, same-day appointments introduced across the country by Walgreens to ensure ease of COVID-19 vaccine access. Pharmacy Times . May 3, 2021. Accessed June 14, 2021. https://www.pharmacytimes.com/view/mobile-clinics-same-day-appointmentsintroduced-across-the-country-by-walgreens-to-ensure-ease-of-covid-19-vaccine-access
21. Coppock K. Pharmacies extending Friday hours in June to increase access to COVID-19 vaccination. Pharmacy Times . June 10, 2021. Accessed June 14, 2021. https://www.pharmacytimes.com/view/pharmacies-extendingfriday-hours-in-june-to-increase-access-to-covid-19-vaccination
22. Weitzman D. The importance of provider status for pharmacists. Pharmacy Times . November 17, 2020. Accessed May 25, 2020. https://www.pharmacytimes.com/view/the-importance-of-provider-status-for-pharmacists
23. Face-to-face with community pharmacies. National Association of Chain Drug Stores. Accessed June 15, 2021. https://www.nacds.org/pdfs/about/rximpact-leavebehind.pdf
24. Understanding the federal retail pharmacy program for COVID-19 vaccination. CDC. Updated April 12, 2021. Accessed May 25, 2021. https://www.cdc.gov/vaccines/covid-19/retail-pharmacy-program/index.html
25. Hopper L. One-third of neighborhoods in big U.S. cities have been ‘pharmacy deserts.’ USC News. May 3, 2021. Accessed May 25, 2021. https://news.usc.edu/185748/pharmacy-deserts-american-cities-healthdisparities-usc-research/
26. CVS Health builds on community-based strategy to address COVID-19 vaccine education and equity. CVS Health. February 19, 2021. Accessed May 25, 2021. https://cvshealth.com/news-and-insights/press-releases/cvshealth-builds-on-community-based-strategy-to-address-covid-19
27. Shen SC, Dubey V. Addressing vaccine hesitancy: clinical guidance for primary care physicians working with parents. Can Fam Physician. 2019;65(3):175-181.
28. Vyas D, Galal SM, Rogan EL, Boyce EG. Training students to address vaccine hesitancy and/or refusal. Am J Pharm Educ. 2018;82(8). doi:10.5688/ajpe6338
29. Misconceptions about seasonal flu and flu vaccines. CDC. May 21, 2021. Accessed May 25, 2021. https://www.cdc.gov/flu/prevent/misconceptions.htm
30. Universal influenza vaccine research. National Institutes of Health. September 5, 2019. Accessed May 25, 2021. https://www.niaid.nih.gov/diseases-conditions/universal-influenza-vaccine-research
31. Rawson SJ, Conway JH, Hayney MS. Addressing vaccine hesitancy in the pharmacy. J Am Pharm Assoc. 2016;56(2):209-210. doi:10.1016/j.japh.2016.02.008
32. Anderson EL. Recommended solutions to the barriers to immunization in children and adults. Mo Med. 2014;111(4):344-348.
33. Hippensteele A. Mobile clinics, same-day appointments introduced across the country by Walgreens to ensure ease of covid-19 vaccine access. Pharmacy Times. May 3, 2021. Accessed June 14, 2021. https://www.pharmacytimes.com/view/mobile-clinics-same-day-appointmentsintroduced-across-the-country-by-walgreens-to-ensure-ease-of-covid-19-vaccine-access
34. Preparing for questions parents may ask about vaccines. CDC. April 11, 2018. Accessed June 14, 2021. https://www.cdc.gov/vaccines/hcp/conversations/preparing-for-parent-vaccine-questions.html
35. Mobile vaccination resources. CDC. March 16, 2021. Accessed June 14, 2021. https://www.cdc.gov/vaccines/covid-19/planning/mobile.html
36. Health literacy: culture and language. CDC. April 20, 2021. Accessed June 16, 2021. https://www.cdc.gov/healthliteracy/culture.html
37. Edwards KM, Hackell JM; Committee on Infectious Diseases, The Committee on Practice and Ambulatory Medicine. Countering vaccine hesitancy. Pediatrics. 2016;138(3):e20162146. doi:10.1542/peds.2016-2146
